Transcatheter replacement of the aortic valve (TAVI/TAVR) is an increasingly common alternative to open surgery for patients with symptomatic severe aortic stenosis across risk levels. This may be due to the fact that associated complications have continued to fall as operators gain more experience and technology and techniques improve;1 however, no medical procedure is entirely without risk.
For TAVI and TAVR, arrhythmias and conduction disturbances—including postoperative atrial fibrillation, new-onset left bundle branch block (LBBB), and various degrees of atrioventricular (AV) block—are medical complications, with many patients requiring permanent pacemaker implantation (PPI). In fact, PPI is the most common complication of TAVI, occurring in 13% of cases, according to one estimate.2
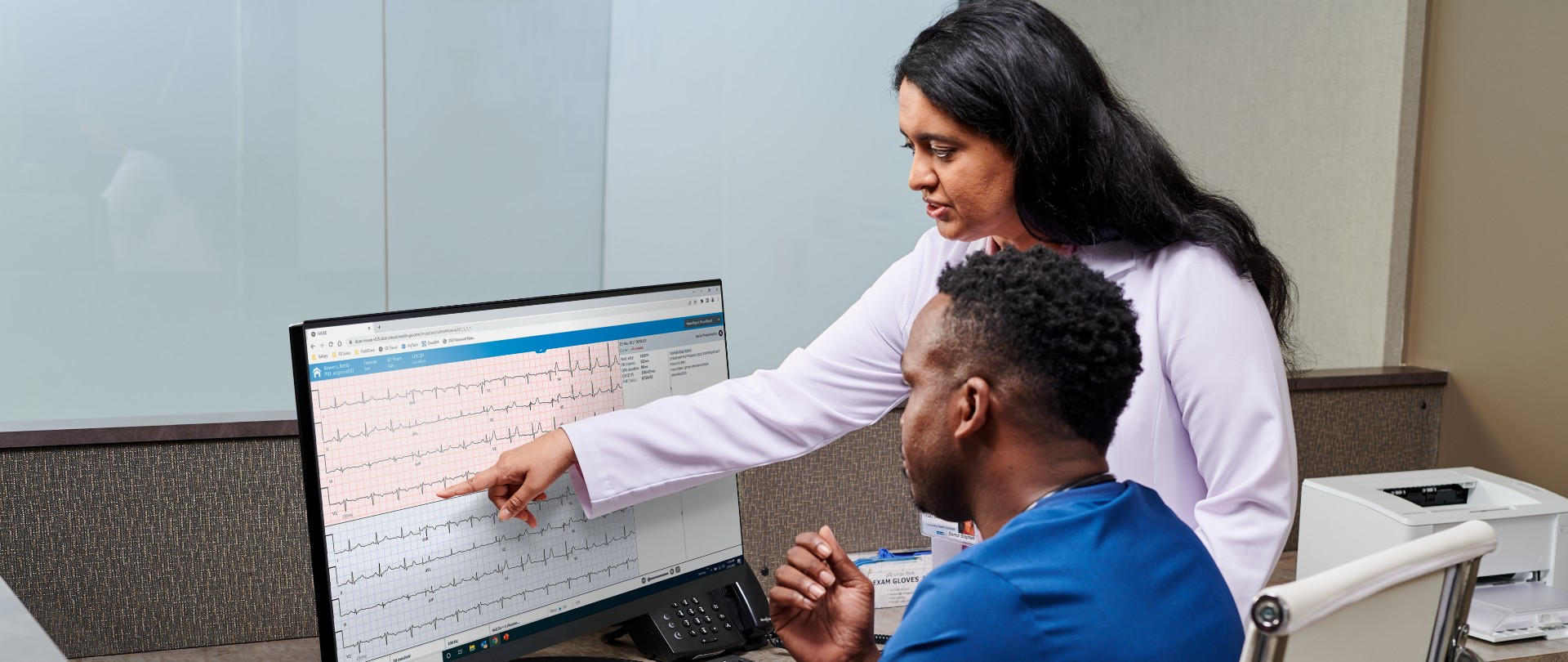
As the procedure can have such a meaningful impact on the heart's electrical system, with conduction disturbances that can be picked up days or even months later, the ECG takes on a prominent role in monitoring for complications immediately following TAVI and on an ongoing basis.3 An expert consensus decision pathway from the American College of Cardiology (ACC) calls for an echocardiogram and ECG even before hospital discharge.4 After discharge, the ECG should be included in a routine 30-day follow-up appointment to look for complications and then annually thereafter.
"In addition to echocardiography, periodic ECG monitoring is recommended for detection of asymptomatic AF and because heart block or other conduction defects can occur late after TAVR," according to the ACC, which notes that a requirement for PPI can emerge beyond the first 30 days.
New Permanent Pacemaker Implantation after TAVI
A requirement for PPI has been a common complication since the advent of TAVI. "Because this is felt to be due to a direct effect of the prosthesis on the conduction system, one would expect the rates to be highest in the periprocedural period," researchers say in an editorial discussing the results of the CoreValve US Pivotal Trial.5 In a paper describing the three-year results of that trial,6 much of the need for PPI indeed had emerged by 30 days (19.8% with TAVI and 7.1% with surgery), but the rate continued to increase as time went on: one year (22.3% vs 11.3%), two years (25.8% vs 12.8%), and three years (28.0% vs 14.5%).
The researchers point out that about 22% of patients entered the trial with an existing pacemaker, meaning about half of trial participants would require PPI by three years. In addition to impacts on cost, resource use, and long-term ventricular function, this "gradual yet tenacious need for pacemaker implantation beyond the initial 30-day period may also have implications for routine screening protocols in patients receiving TAVR," they say.5
In another editorial, researchers explain how the implantation of a transcatheter prosthesis in the aortic valve can lead to a need for PPI, pointing out that the presence of right bundle branch block (RBBB) before the procedure is the strongest predictor of new-onset high-grade AV block.7 "This is because compression from the TAVR prosthesis on the membranous septum and interleaflet triangle between the right and noncoronary cusps threatens mechanical insult to the closely approximated left bundle branch, thereby risking a compounding of the baseline conduction deficit," they say. "Even with normal preprocedural conduction, new onset left BBB (LBBB) induced by TAVR may herald higher grade atrioventricular block via this mechanism and confers a 2-fold increased risk for early PPI."
Despite these insights, the authors express surprise about the relative dearth of knowledge about how electrical conduction disturbances evolve in the weeks after TAVI, which has spurred much variability in the use of PPI—and in the management of conduction disturbances more generally.
Managing Conduction Disturbances after TAVI
The lack of consensus on how to manage conduction disturbances after TAVI led the Journal of the American College of Cardiology (JACC) to bring together an expert panel of interventional cardiologists, electrophysiologists, and cardiac surgeons to formulate some initial guidance.8
After defining various possible conduction disturbances after TAVI—including RBBB, LBBB, left anterior and left posterior hemiblock, intraventricular conduction disturbance, and various degrees of AV block—the group proposed a strategy for clinicians. The following are condensed, paraphrased recommendations from the JACC:
- Patients should undergo a preprocedural risk evaluation for conduction disturbances, and operators should consider procedural modifications to minimize the risk of these complications.
- Clinicians should use telemetry during the procedure, and they should perform a 12- or 6-lead ECG at the end.
- If there are no ECG changes and no pre-existing RBBB, temporary pacing is not necessary, but telemetry should be used for 24 hours (or at least overnight)—such monitoring can pick up postoperative atrial fibrillation and other issues.
- For patients with no ECG changes but with pre-existing RBBB or for those with baseline ECG changes (including changes in conduction disturbances, new-onset LBBB, or high-degree AV block/complete heart block), clinicians should opt for temporary pacing for 24 hours (or at least overnight), with consideration of stopping earlier if the ECG changes resolve.
- Options then include additional evaluation or observation accompanied by temporary pacing, electrophysiological (EP) studies, or continuous ECG monitoring; PPI; or no further evaluation or observation.
The JACC scientific expert panel stresses that this strategy should be vetted in future studies: "It should be considered a work in progress... A compromise between the increasing pressure toward a minimalist approach including early discharge of TAVR recipients and the potential risks associated with overly-precipitous clinical decision-making in this context has been taken into consideration throughout the entire document."
A more standardized approach to dealing with these complications, however, may pay dividends in terms of the management and outcomes of affected patients, they add.
What's Happening in Practice?
A recent survey from the European Heart Rhythm Association (EHRA) provides insights into whether more uniformity has emerged around the management of conduction disturbances after TAVI.9 A 25-item online questionnaire was sent to EHRA electrophysiology research network centers, with 117 physicians responding.
Overall, 63% of centers had a standardized protocol in place to manage advanced conduction disorders like LBBB or AV block after TAVI. The most common management strategy for patients with new-onset or pre-existing LBBB was telemetry after the procedure (79% and 70%, respectively). There was variation in the duration of telemetry after new-onset LBBB, however, 48 hours was the most frequent duration; nearly half performed such monitoring for 72 hours or longer.
Moreover, among patients with new-onset LBBB, the ECG-measured his-ventricular (HV) interval that spurred implantation of a permanent pacemaker varied across centers, with a threshold > 75 ms being the most popular.
The findings reflect continuing heterogeneity in practices. "There is considerable room for improving the management of patients with conduction disorders after TAVI, and a clear need for dedicated management protocols in TAVI patients covering monitoring and risk assessment for HAVB [high-degree AV block] based on EP studies, clinical risk factors, and/or ILR [implantable loop recorder] placement," the authors state.
Although this survey underscores the need for more standardization in practices when it comes to detecting and managing conduction disturbances after TAVI, the ECG will clearly remain a key player moving forward.
Resources:
1. Mach M, Okutucu S, Kerbel T, et al. Vascular Complications in TAVR: Incidence, Clinical Impact, and Management. J Clin Med. 2021;10(21):5046. Published 2021 Oct 28. doi:10.3390/jcm10215046
2. Auffret V, Puri R, Urena M, et al. Conduction disturbances after transcatheter aortic valve replacement: current status and future perspectives. Circulation. September 2017;136(11):1049-1069.
3. TCTMD. Studies zero in on delayed conduction problems after TAVI. TCTMD.com. https://www.tctmd.com/news/studies-zero-delayed-conduction-problems-after-tavi. Accessed April 27, 2023.
4. Otto CM, Kumbhani DJ, Alexander KP, et al. 2017 ACC expert consensus decision pathway for transcatheter aortic valve replacement in the management of adults with aortic stenosis: a report of the American College of Cardiology task force on clinical expert consensus documents. Journal of the American College of Cardiology. March 2017;69(10):1313-1346. https://www.jacc.org/doi/10.1016/j.jacc.2016.12.006
5. Kumbhani DJ, Banerjee S. 3-year results of a TAVR trial in high surgical risk patients. Journal of the American College of Cardiology. June 2016;67(22):2575-2577. https://www.sciencedirect.com/science/article/pii/S0735109716324056
6. Deeb GM, Reardon MJ, Chetcuti S, et al. 3-year outcomes in high-risk patients who underwent surgical or transcatheter aortic valve replacement. Journal of the American College of Cardiology. June 2016;67(22):2565-2574. https://www.sciencedirect.com/science/article/pii/S0735109716016909
7. Gulati R, Wang A. Left bundle branch block before transcatheter aortic valve replacement: is there a risk? Circulation: Cardiovascular Interventions. November 2018;11(11):e007361. https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.118.007361
8. Rodés-Cabau J, Ellenbogen KA, Krahn AD, et al. Management of conduction disturbances associated with transcatheter aortic valve replacement: JACC scientific expert panel. Journal of the American College of Cardiology. August 2019;74(8):1086-1106. https://www.jacc.org/doi/10.1016/j.jacc.2019.07.014
9. Badertscher P, Knecht S, Zeliković I, et al. Management of conduction disorders after transcatheter aortic valve implantation: results of the EHRA survey. EP Europace. July 2022;24(7):1179-1185. https://academic.oup.com/europace/article/24/7/1179/6554408